Reorienting to the smart health experience
As the health system becomes smart, the defining narrative of the industry will shift to that of optimizing experience for both consumers and clinicians. Organizations will reorient around concern for delivering not only clinical sick care but also end-to-end well care that is personal and empathetic. Digital technology will provide the tools.
At the heart of this shift lies underlying assumptions on what shapes the production of health and whether the current model of health care is suited to modern-day needs. The supply model of health is generally a siloed, waterfall model, which delivers poor experiences. The new world of experience is driven by a digitally enabled, demand-led, agile model of health care.
Constant reinvention to meet consumer and clinician needs means finding the balance between what has worked in the past and what needs to be done for the future. As Kristi Henderson, DNP, SVP Center for Digital Health & Innovation, Optum, United Health Group says, “We have to keep listening to our customers and keep evolving our platforms, products, processes, tools and services to match those needs. And we’ll never be done.”
Daniel Kraft, MD, Founder and Chair of Exponential Medicine, points out that just digitizing analog processes is not the answer saying, “A digital fax machine does not move the needle, rather, it entrenches the old way of doing things.”
To remain relevant in a fast-changing environment, health care organizations will need to tackle the duality of growth: taking care of the business of today while innovating to build the health system of tomorrow. (Figure 1, The Duality of Growth) In the context of smart health, this means being clear about how value is created through balancing innovation and exploring improving experiences with the need for operational effectiveness. For many organizations, this shift toward engagement and optimized experience may be highly disruptive to a status quo built around utilization and volume.

EY’s research found three essential shifts needed to build and elevate a future-forward, smarter health experience:
- Getting the health experience right means moving beyond just delighting in the moment to systematically paying attention to what matters
- To realize a smart future, all elements of a health ecosystem must work in concert
- Smarter health experiences create long term trust and elevate the empathetic human touch

Chapter 1
Essential shift 1: Getting the health experience right
Move beyond just delighting in the moment to systematically paying attention to what matters.
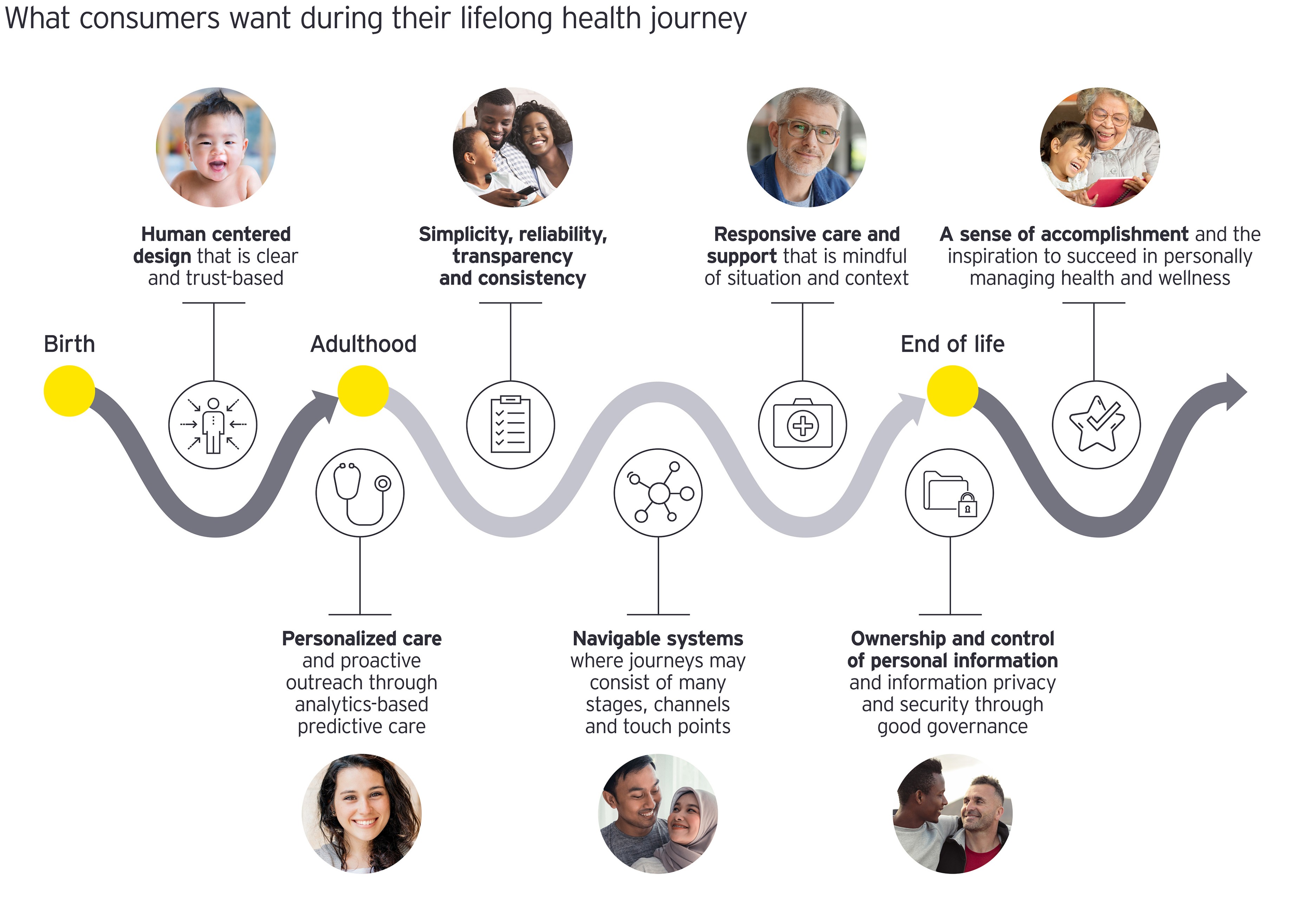
What constitutes good health care experiences, how to achieve them and why they are important is not widely shared or clearly understood. And yet, these are some of the most important strategy questions facing health systems today. How an individual perceives health is unique and intensely personal, and health outcomes are shaped by many nonmedical factors, including education, income and cultural perspectives.
Industry executives interviewed were confident that, in the future, the health industry will be built upon a deep understanding of benefit arising from improving the end-to-end health and wellness care experience, especially in keeping these three factors in mind:
1. People at the heart
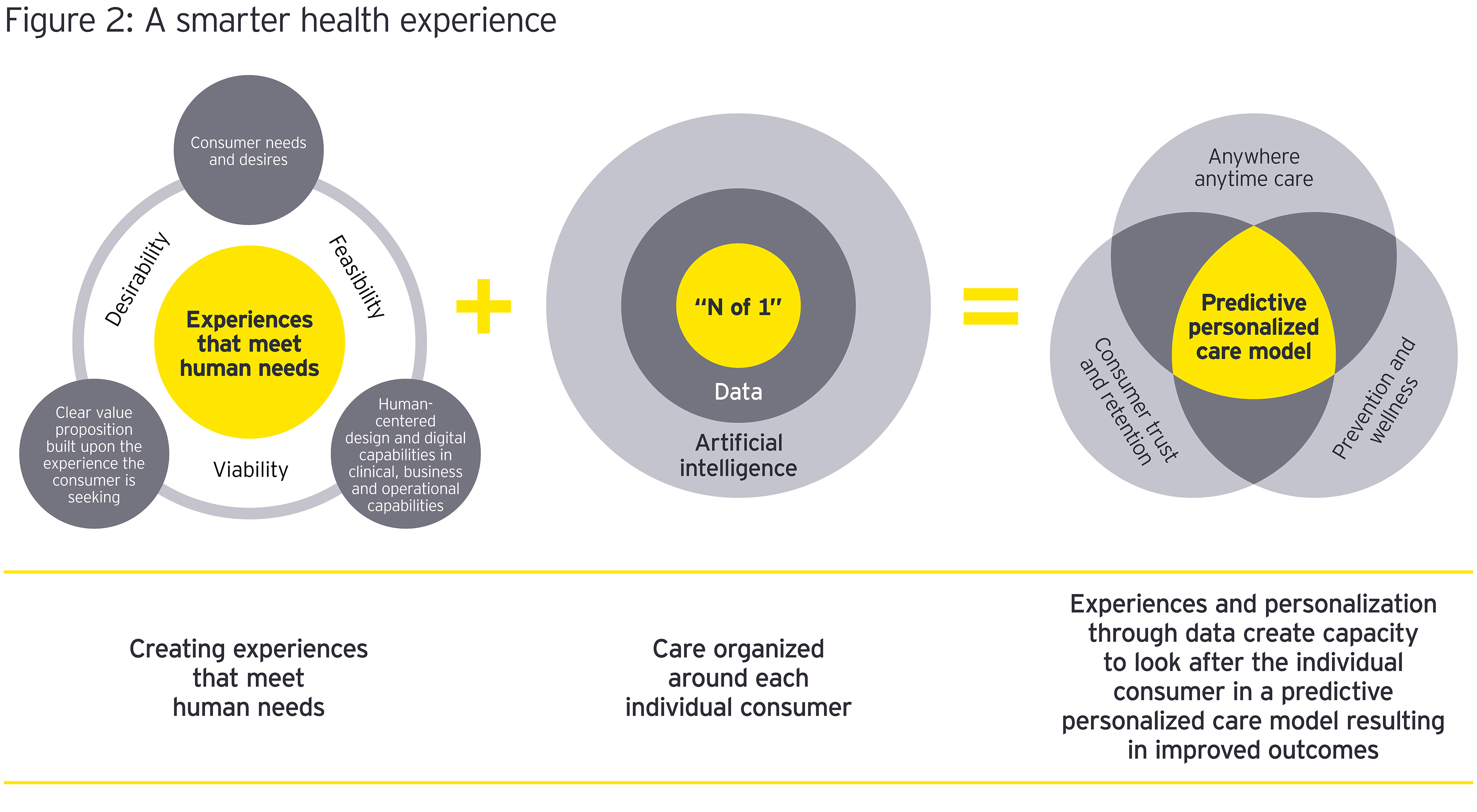
Getting the experience right means valuing people for who they are and understanding each person’s unique set of needs. For consumers, good experience is highly personalized, proactive and engaging care, tailored to them, as an “N of 1.” For clinicians, it is meaningful engagement with their work in a low-friction, modernized and inspirational environment.
A good health care experience is highly nuanced. The strategic challenge is creating an emotional connection between patient and organization over the health journey. Interviewees emphasized the creation of trust as a fundamental pillar of this relationship. A seamless digital experience can make the difference in consumer loyalty and retention, and the future lies in building digital services that add value. Rachel Dunscombe, CEO, NHS Digital Academy, stresses the importance of a strategy-led approach, saying, “It’s a wider context than just delighting in the moment. We need a systematic approach to getting it right. A nuanced and subtle focus on continual optimization of experience will ensure ongoing patient engagement and create optimal health care.”
2. Personalized and precise
Those interviewed clearly saw that there is no one “best” experience. Rather, an optimal experience aligns consumer need with the right resources, in the right setting. As Daniel Kraft observes, today’s health care system is designed as one-size-fits-all. Health systems need to “pay attention to matching the consumer, just like we do in precision medicine – right drug, right dose, right combination,” Kraft says. “When you think about it, it is precision engagement, in a sense to ‘get it right’ — there’s no one-size-fits-all. Ideally, this will lead to precision digital health that matches the patients age, culture, language, education, personality and incentives.”
When you think about it, it is precision engagement, in a sense to ‘get it right’ – there’s no one-size-fits-all.
To this end, data and analytics are important tools of discovery and for crafting personalized responses. This includes known information about an individual’s health, but also information on diet, activity levels and lifestyle factors. ‘Omics data should be added as it comes onstream so that treatment and predictive health behaviors are tailored to the N of 1.
3. Time and design
Eric Bricker, MD, Chief Medical Officer, AHealthcareZ, believes that the three things necessary for good patient experiences are the matching of clinical expertise and patient need, sufficient time to deal with the issue, and clinicians with access to the right tools. As he says, “It takes time … if you’ve ever tried to fix a faucet in your house, it takes time. So, if you’re only spending seven minutes a visit … it doesn’t matter if you have all the expertise in the world, it still takes time.”
This mismatched problem of expertise, time and tools, or the capacity to tailor personalized care, is one of the key problems in the pathway to becoming truly consumer centric. Patient journeys can be complex, and even more so as dual streams of offline and online services come into play. Orienting around the consumer calls for decoupling care from location and making it feel seamless and unified for the patients. (Figure 2, A Smarter Health Experience) The task is one of designing the system to meet the needs of the consumer rather than bending the consumer to the system. As one executive notes, “At the end of the day, good health care provision is not fully online or fully offline, it is a seamless experience that we need to provide.”
How can health care organizations transform into truly consumer centric organizations?
Consumers bring to health care the same expectations of digitally enabled solutions they enjoy in other industries, such as travel, transportation, financial services and retail. To become consumer centric and experience-led requires a rethinking of the vision and strategic intent of the enterprise. Neil Sorrentino, PhD, Chief Global Strategist, Bumrungrad Hospital, Thailand, suggests that this demands being clear about the principal value proposition of the organization and focusing resources and energy around consolidating and extending brand equity and brand visibility. “You have to be thinking differently, how to distinguish yourself and how you get patients’ attention,” he said.
At Bumrungrad Hospital, the organization has worked through a process of rethinking how it looks at patients, pivoting from being internally oriented to becoming outwardly focused. This has meant homing in on the experience the customer is looking for and using technology to remove irritants to customers to make the health experience better. Turning thinking around has sparked a raft of new initiatives around social and digital connectivity with patients; the creation of new services in the wellness and lifestyle domains; attuning communications to generational preferences; and reaching new markets through co-branding with unorthodox partners, such as with a large retailer’s loyalty program.
You have to be thinking differently, how to distinguish yourself and how you get patients’ attention.
In the long run, many of the interviewees expect that health organizations will come to recognize the value of an unwavering focus on consumer experience. To achieve this means building next-generation operating models that apply digital capabilities to clinical, business and operational processes. One executive described how using AI-driven analytics effectively dealt with a costly back-office problem achieving operational efficiencies and improving customer satisfaction, saying, “So this use of the data, while it’s not as sexy as using radiology data or things like that, it’s a very programmatic use of data [that] helps out operations, as well as patient satisfaction.”
However, many mitigating factors exist, including the challenges of organizations that have grown by acquisition and thus have federated operations of considerable complexity. Other factors noted included multisite networks with differing levels of digital maturity, the vast variations in physician employment and compensation models, the extent to which the organization “owns” the full spectrum of the patient journey and the thorny question of “who pays” for experience. These all influence the ability to achieve the scale, scope and sustainability necessary to consistently deliver exceptional patient and clinician experiences.
Central to this shift: Trust
Trust is the biggest prerequisite for harnessing the power of digital transformation in health care. Trust and loyalty drive experience, and, while many in the health industry work to improve a patient’s health, the bond of trust that forms between patient and provider is central. The technologies that will get health care to an anywhere, anytime system already exist; patient engagement tools, virtual care, smart homes and AI-powered analytics will give people the means to manage their health, lifestyle choices and chronic conditions in vastly different ways.
Trust, however, has to be earned. The patient experience is the starting point, and the design intent is to transform the look and feel of services for a better care experience and sustained loyalty, or “stickiness.”
Smart health technology, along with the human touch, offers opportunities to change care delivery in ways that matter to both consumers and clinicians. And from an enterprise perspective, automation and system process redesign will streamline middle- and back-office workflows so that clinicians can spend more time caring for patients.
What this shift means:
Health care should reorganize around experience optimization in a technologically advanced environment.
As a result:
Health systems deeply understand the utility gained from improving the end-to-end health care experience for both consumers and clinicians. Based upon this, new business archetypes and paradigms will emerge that will be based upon an organization’s proficiency in leveraging ecosystems, technology and data. In a highly competitive market, customer stickiness is key, and the depth of engagement will be built upon great experiences.

Chapter 2
Essential shift 2: Realizing a smart future
All elements of a health ecosystem must work in concert.
Delivering smarter health care and well-being at scale is immensely complex, especially in an industry with multiple players and one that, until the COVID-19 pandemic, was notoriously slow to change. As digital transformation within the health care system gathers pace, smart ecosystems will need to emerge and create new pathways by which to organize and deliver health care. These ecosystems will be built on these elements:
1. Co-creation and iteration
Recognizing the complexity of having all elements work together in an ecosystem, several people we spoke with stressed the need for co-creation with users and a willingness to iterate rather than to get it right the first time. Systemic design and architecting for expected future changes in health care, such as being able to incorporate emerging fields of ‘omics data, are important. As Daniel Kraft notes, “If we build a platform in 2021, it may not be the platform that’s going to work in 2030, but we need to architect it so that it’s somewhat future-proofed.”
The health system needs to evolve from the current situation of siloed point solutions. Apps, wearables, devices and portals bring multiple digital touchpoints that can create even more noise in an already complex patient journey. Sam Marwaha, Chief Commercial Officer, Evidation Health, points out: “A world in which there are thousands of apps is not friendly to an individual. The answer to engagement lies in building better platform environments that support the individual’s health journey.” He suggests that a better solution for the industry overall is for something like a “Spotify for health care” to emerge as an enabler of the underlying platform, explaining: “It’s a clearing house, to a certain extent, for generating evidence-incorporating measures that matter to patients, validating it in the right sort of way, and then making that evidence actionable at the point of intersection between the clinician and patient.” This requires the health industry to move away from facility-centric models to evidence-supported management plans based on person-generated health data.
The solution for the health industry overall is something like a Spotify for health care.
2. Comprehensive platforms
Different types of platforms are emerging in response to key areas of demand, such as convenience care, specific condition management, virtual telehealth, integrated virtual and physical care, and retail health.
The digital front door, or one-touch digital entry points between a consumer and a health system, is a natural fit with platforms orchestrating a network around the person. Digital front doors present a gateway to connect and stay with the patient throughout his or her journey. They also enable a more flexible clinical model — one that shifts care to the right type of provider at the right time, as organizations use AI to adjust clinical staffing models based upon need and demand surges. “Platforms are really, really, really important. But they'll fail without having the right governance,” says Rachel Dunscombe, CEO NHS Digital Academy.
3. Creative partnerships
Industry executives saw that orchestrators of smart ecosystems may well come from outside the health industry (e.g., global brands running digital platform businesses). Partnerships are already emerging between consumer, tech or electronics companies and leading health industry players that blend the technical capabilities of one partner with the service and health care expertise of another. Daniel Kraft drew an analogy with an orchestra, saying that the challenge was to, “create an orchestra with interchangeable bits … and get the big players and small players to tune up in the same key.”
Platforms are really, really, really important. But they'll fail without having the right governance.
4. Solid governance
Governance systems that deliver trust are seen as a critical success factor. In particular, good governance around how platforms capture, store and give access to data is necessary to establish user trust (both consumer and clinician) and for privacy and security to be maintained.
As the focus of health systems moves toward supporting wellness — anytime, anywhere — an open platform environment is required to connect and share permissioned data, at scale, within and among enterprises and systems. An open platform is one that “separates content and technology and is vendor neutral, distributed and modular.” 3 Types of platforms that are likely to become dominant in the future will include several key features of a technology architectural infrastructure, an analytics and intelligence layer, and a user engagement interface.
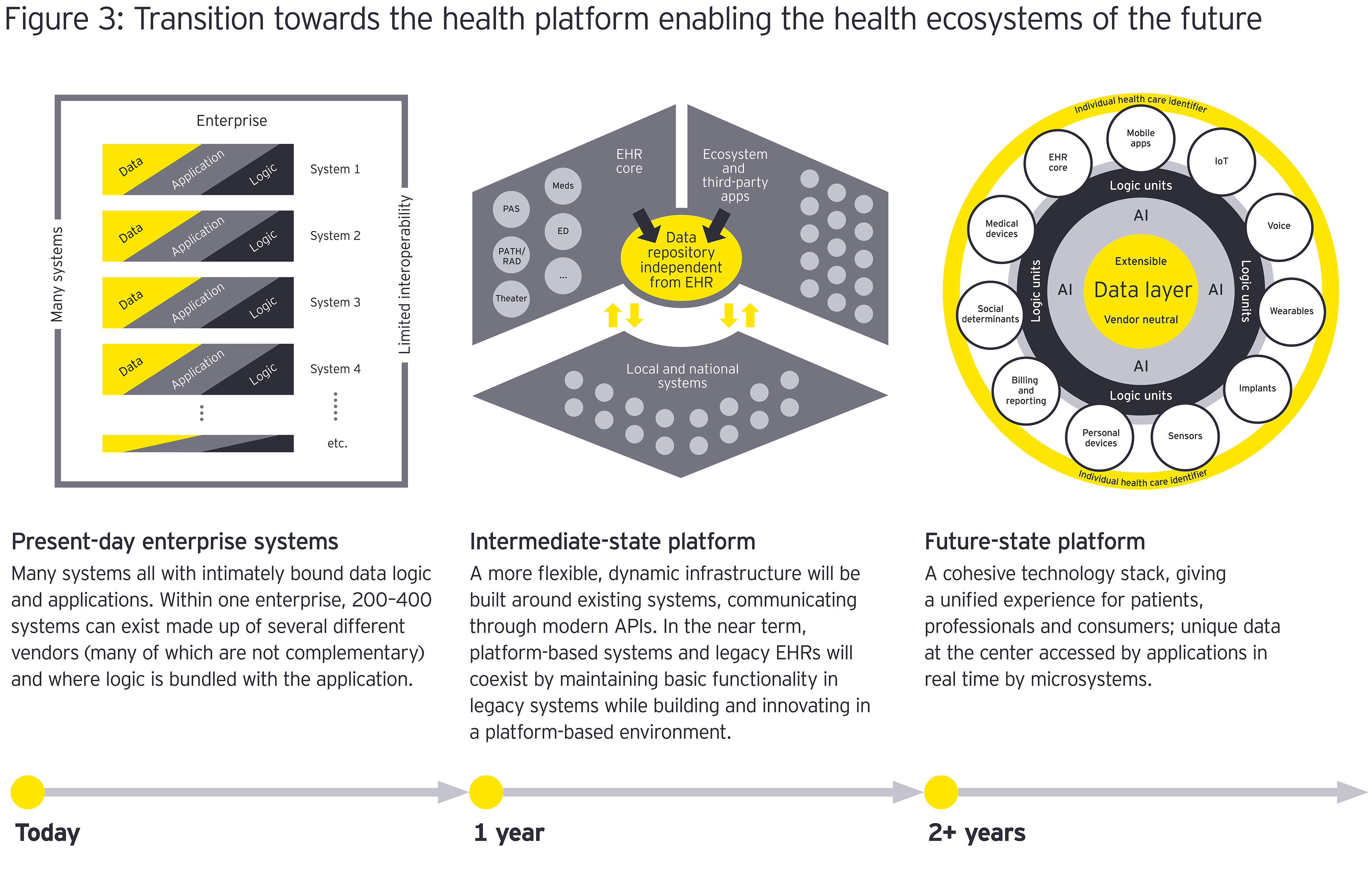
The patient experience moves from siloed systems with little ability to share information to a cohesive technology stack and a networked infrastructure that delivers a unified experience.
“When I think about a super-platform that supports care for life … it must have contextual intelligence to meet the customers’ expectations and care needs,” says Kristi Henderson, DNP, SVP Center for Digital Health & Innovation, Optum, United Health Group. “How we use the data and the AI applied to it must be balanced and masterfully orchestrated with human interaction and skilfully placed automation to build a trusted relationship with ongoing engagement.”
When I think about a super-platform that supports care for life … it must have contextual intelligence to meet the customers’ expectations and care needs.
Central to this shift: Interconnected ecosystems
As health care becomes smarter, the industry will transition from siloed and transactional to one where all elements of the health care ecosystem work in concert. Technology in all of its various forms will create common platforms to provide advanced support across all tasks and insights relevant to a clinical encounter or patient journey. Ecosystems that connect all players of relevance to a patient are built upon advanced architectural integration of data and intelligent analytics of that data to create informed insights to manage care. The intuitive nature of data supports the application of AI and machine learning to truly predict the right treatment protocols, what keeps people healthy and what will nudge healthier behaviors.
Policy and regulation deliver the essential checks and balances of good governance necessary to underpin a connected ecosystem. As connectivity becomes more central to health care, regulators will continue to take a strong stance on the need for interoperable yet secure data, including ensuring that consumers have control over their health information. Gaining consumer and clinician trust is critical, particularly when it comes to the safety, validity and integrity of the data generated.
What this shift means:
Platforms form function al ecosystem(s) to deliver network effects, value and benefit in new combinations of the growing web of industry stakeholders: providers, payers, new entrants and others, such as financial institutions, housing, employment and social support services.
As a result:
A highly interconnected health ecosystem providing a superior user experience that accommodates individual preferences, uplifts the end-to-end experience and connects across the care continuum. Health, wellness and prevention are optimized through personalized therapy that is data driven.

Chapter 3
Essential shift 3: Building trust with smarter health
Smarter health experiences create long-term trust and elevate the empathetic human touch.
As the health care model changes from siloed to patient-centered, digitally enabled and demand-led, there will be growing pains: persuading consumers, clinicians and those charged with governance to adjust business and clinical processes to get the right care delivered at the right time, all of the time, in ways valued by the consumer.
Kristi Henderson spoke of the importance of long-term trusted relationships that are the foundations of personalized care. Drawing upon a care team’s shared knowledge of an individual and their personal network is how N of 1 interactions can become scalable. However, as she says, “It’s common sense but it’s not done because it’s hard and takes a lot of work. It’s an intentionality that’s not built into our operating model which is based upon appointments 15 minutes apart.”
Knowing the unique customer and enabling him or her to define preferences heightens the importance of design thinking in improving the clinician and consumer user experience across health care settings. Daniel Kraft emphasizes the importance of simplification, saying, “People don’t always want to be reminded of their health or be bugged” and that, for clinicians, “No one wants to jump through a bunch of hoops to collect data … the clinician wants insights and actionable information, not just raw sleep data.”
Several people spoke of issues with user experience in health care, especially about complex health IT systems. Transforming the experience is not just an issue of end-user satisfaction. It is achieving the right balance between users customizing how they consume information and the safety net of standards.
Rachel Dunscombe describes this well:
“We can't infinitely personalize and remain safe. What I’m asking for is both standardization and variation at the same time. Standardization to a set of ways of working, for example how blood pressure or renal function are displayed. But then personalization for the clinician to match their operating practices such as how they arrange the widgets on the screen to consume that experience. It's that combination of warranted variation that gives a great experience and standardization that brings safety.”
To this end, co-design with clinicians, patient and consumer groups is a hallmark of human-centered design, designing with and for people. The best outcomes arise through a participatory co-design process, where health care consumers and workers imagine what a better experience could look like for everyone.4 For example, co-design can focus on elements of education, access to data, interpretation of results and predictive insights to improve well care. In addition, agile design of smart buildings and virtual services, including modular facilities, hardware, software and networks, is required to meet future demand as new technologies, innovative new care models and different ways of working come into play.
Measuring consumer centricity
Increasingly, patient experience is a central outcome for health care organizations alongside clinical effectiveness and safety. Measuring and improving patient experience are vital steps in understanding and improving the quality of care. Value for organizations arises through clinical processes, along with a robust business case that links patient experience to financial performance, brand and reputation, patient loyalty, and employee satisfaction and retention.5, 6, 7, 8
Industry executives hold a strong interest in understanding experiences in the moment, as well as customer trust and loyalty. The generation of trust is important for brand equity and reputation, and for how consumers make decisions on where to seek care.
The customer experience metric, Net Promoter Score (NPS), is used by many interviewees; however, the NPS is only one measure used to gauge consumer experience. Other measures used included customer satisfaction surveys, mystery shopper research and benchmarking performance against peers.
Some organizations track whether patients are using the digital tools provided (e.g., hospital apps, remote monitoring or patient portals). This is important for clinical reasons but also for future data mining of customer activity, customer preferences and creating more finely targeted experiences for patients. Looking outside of the health industry to see how others are evolving how they look at and measure trust (such as financial services) may be one way the health industry can continue to evolve how it understands and builds on improving patient trust.
The advent of digital health at scale raises the bar on consumer engagement and loyalty. Patients value the interpersonal aspects of their health care experiences and need a reason to stay, especially in a digital health ecosystem where switching becomes easier. Digital tools make it easier for consumers to find alternatives and switch to get what they want. This raises interesting issues around the cost of switching — to what extent does exceptional service counter the attractiveness of care that may be cheaper or easier to access?
Central to this shift: trusted technology
As health systems become highly digitized and connected, integral to this is the circle of care or the personal trusted network that keeps people healthy and well. Technology is an enabler rather than the end game. It is the experience component that ultimately makes it possible to deliver better, smarter care. If experience is not thought about up front, then pockets of success are likely, when what is needed is wholesale improvement.
Other factors demand attention, such as who pays for experience — the consumer or the payer? Or should the provider regard it as a cost of doing business? Another key factor is finding the right blend of talent with the skills and capabilities to support a data-driven, consumer-centric smart ecosystem.
What this shift means:
The central role that health and wellness plays in people’s lives shows that the route to better health is through individualized and targeted treatments rather than a one-size-fits-all approach.
As a result:
Health systems invest time in bringing people together with the technologies and move from being digitally naïve to engaging and empowering consumers and clinicians through health and well-being as an everyday-lived experience.
A vision of a better, more engaged health industry
Leading industry executives share a strongly held vision that, in the future, health care will reorient around a truly shared sense of purpose between the consumer and the health enterprise.
EY’s view is that industry transformation will be built upon innovations and interconnected ecosystems that all work in concert to make health care simpler and more seamless. This is especially true for those that succeed in gaining and sustaining consumer engagement with their health and wellness across their lifespan.
It is clear that what makes for a good health experience is highly nuanced, and the creation of trust between the consumer and health care organization is foundational. Trust has to be earned, through close and supportive relationships that drive deep engagement and are built upon great experiences. Rather than just delighting in the moment, a systematic approach to deeply understanding what matters to people is instrumental in getting the health experience right. To this end, measuring and innovating to improve the consumer and clinician experience are key to enhancing the quality of care and to capturing data for more finely targeted N of 1 care built upon activity, sentiment and preferences.
We are well on the way to creating a digital-first health experience and weaving digital into every aspect of an organization. As such, smart health ecosystems of networked platforms will level-set the health industry in a new space, completely recasting the connectivity between the consumer and health and social systems. For health care organizations, this means reimagining the value proposition around trust and experience-driven engagement in a technologically advanced environment, building a future operating model around a digital-first approach to patient and clinician experience, and enablement of the back office.
Health care will not be transformed overnight. However, opportunities to initiate disruption abound through targeting areas where a focus on experience will make a big difference for the consumer and clinician. Most important is setting sights on the far horizon. Future-proofing through design means avoiding being locked in by the constraints of the business of today. This has only been accelerated by the impact of the COVID-19 pandemic, taking years off the technology adoption timeline.
Internationally, steady progress is being made toward creating ecosystem-style infrastructures built around the timely and relevant exchange of health data. Steps are being taken toward more open and interoperable systems in Estonia,9 the Nordic countries10 and most recently in England.11 While the health models vary, a commonly held vision is that of data that is sufficiently liquid to flow through the system. This data underpins integrated care platforms that incorporate social determinant, sensor and wearable data, along with health information into algorithms, making personalized, smart care experiences possible.
Sheryl Coughlin, PhD, EY Research Consultant and Lead Writer, contributed to this report.
Summary
One of the most important conversations in health care today is about people. Smart health technology offers untold opportunities to connect and care for individuals in unique and highly personalized ways. To reorient and thrive in the smart health system of the future means systematically paying attention to getting the health care experience right.
