PDF version of the report available now
Interested in learning more about the EY Center for Health Equity?
Key insights from EY's 2nd Annual Health Equity Survey
- 500 health equity leaders were surveyed across provider, payer, life sciences, government, and nonprofit and community organizations.
- 73% of respondents expect an increase in prioritization of health equity over the next year.
- The majority expect investments in health equity to increase yet point to competing priorities as a leading barrier for strategy execution.
- Health equity investments have led to quantifiable benefits to both organizations’ bottom line and health outcomes of populations served.
- The top priorities — health equity access and quality, and health equity strategy development — remain consistent with 2023, while the distribution of subsequent priorities points toward an increased focus on addressing downstream outcomes and a decreased focus on impacting upstream social determinants.
- Organizational size by annual revenue is emerging as a surrogate for the perceived maturity of health equity efforts, suggesting the potential role that access to greater resources plays in taking action.
Survey methodology
Advancing health equity remains a social, political, economic and ethical priority. A variety of stakeholders (providers, payers, life sciences companies, government agencies, and nonprofit and community-based organizations) are working individually and in collaboration to improve health outcomes and narrow gaps. A greater understanding of what is being done, what is working, where challenges persist and what trends will inform future progress is needed. The EY Center for Health Equity’s inaugural Health Equity Outlook Report, published in 2023, established a baseline understanding of health equity efforts across the health ecosystem to advance practice. Findings from the 2024 edition of the annual survey, based on responses from 500 health equity leaders across stakeholder groups, provide an updated view of where we are and where we are going in health equity practice. In-depth views are provided of organizations’ current and expected health equity priorities and investments, technology actions and maturity, and workforce and community engagement.
“Health equity is the state in which everyone has a fair and just opportunity to attain their highest level of health. Achieving this requires ongoing societal efforts to address historical and contemporary injustices; overcome economic, social, and other obstacles to health and health care; and eliminate preventable health disparities.”

Chapter 1
Health equity – current landscape, priorities and investments
Organizations are making advancing health equity a priority, but their approaches and areas of focus differ.
Overall, advancing health equity remains a moderate to high priority for most organizations surveyed, with varying levels of investment, leadership, strategic maturity and capabilities to advance identified priorities.
Priorities
The momentum in health equity is expected to continue, as virtually all the organizations (98%) see prioritization staying the same or increasing over the next year.
Chart 2. Health equity as an organizational priority, current and future perspectives
Variation in how health equity is prioritized exists across segments and by size of organization. Government organizations — especially federal organizations, organizations with over $1 billion in revenue and organizations with more mature health equity strategies — were likely to report higher levels of health equity prioritization, compared with peers.
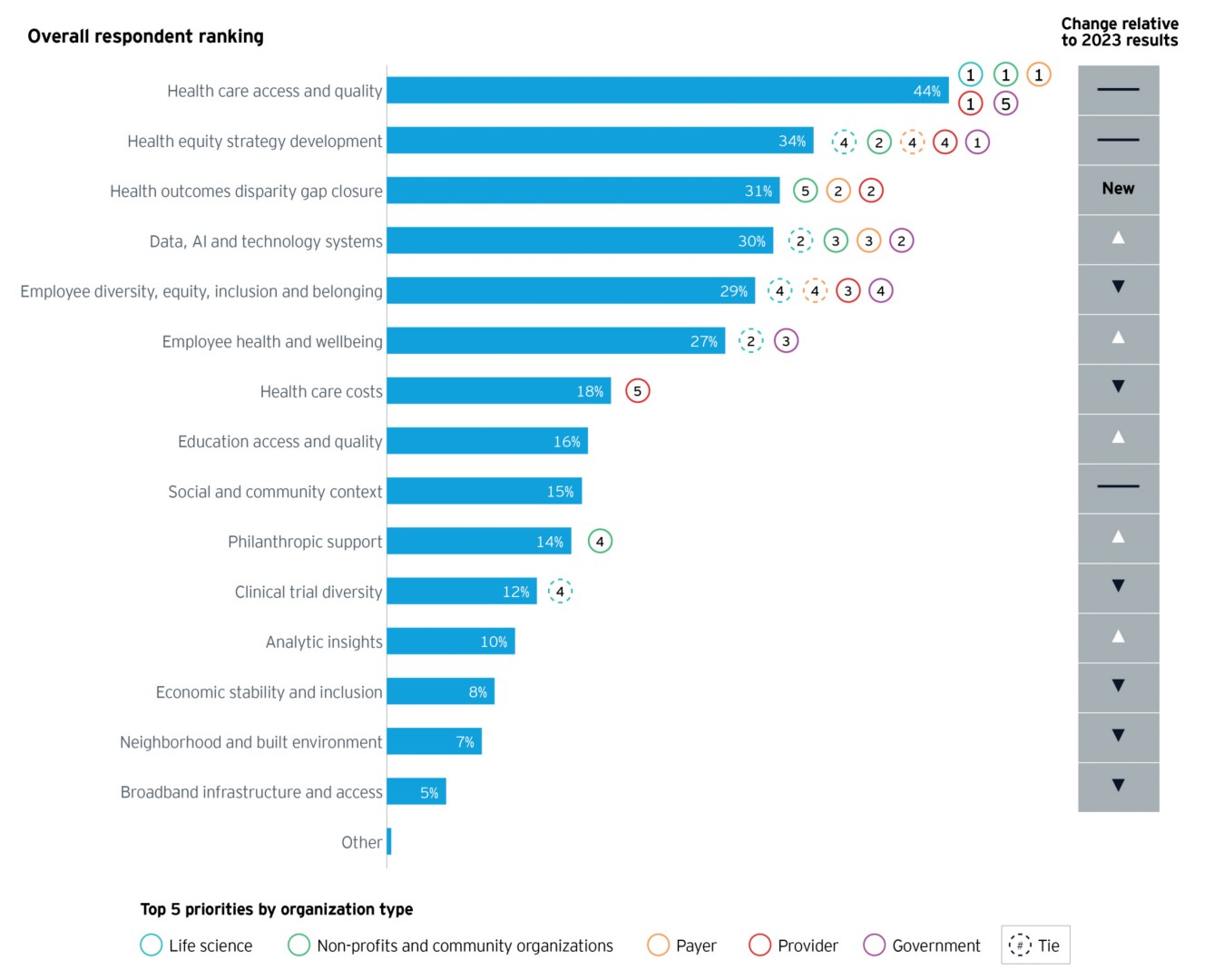
Consistent with last year’s findings, there is diversity in the specific factors and issues prioritized within health equity programs. Health care access and quality remains at the top — with 44% of organizations ranking it in their top three health equity priorities, up from 34% in 2023. Health equity strategy development was cited by roughly a third (34%), consistent with 2023 (33%). Another top area of focus cited was health outcomes disparity closure (31% of organizations).
There was a significant — 50% — increase in those citing data, AI and technology as a priority, while a reduced focus was observed for health care costs and addressing upstream social determinant of health factors such as economic stability and inclusion, neighborhood and built environment, and broadband infrastructure and access.
There was a significant increase in organizations citing data, AI and technology as a top health equity priority.
Chart 3. Evolution of top health equity priorities for the ecosystem and by organization type
Investments and maturity
Most organizations expect that their health equity investments will increase (58%) or stay the same (38%) in the coming year. How organizations invest highlights both priorities and areas where greater maturity is needed to reach goals. Four areas of investment — technology and analytic solutions, design and implementation of health equity initiatives, organizational and workforce development, and ecosystem and community partnerships — are reported to have the highest likelihood of increased investment.
Nearly all expect that their health equity investments will stay the same or increase in the coming year.
Chart 4. Anticipated changes in health equity investments by focus area
Where an organization currently is in its health equity journey also influences the focus of its investment. There are four main stages of health equity maturity that influence stakeholder priorities and spending.
1. Foundational: Health equity identified as an enterprise priority; may or may not have defined health equity metrics and/or initiatives to drive progress.
2. Siloed: Health equity addressed through ad hoc initiatives across multiple parts of the organization; efforts may or may not be aligned to enterprise strategy.
3. Integrated: Health equity addressed through ad hoc initiatives across multiple parts of the organization; efforts may or may not be aligned to enterprise strategy.
4. Sustainable: Health equity strategy embedded and sufficiently resourced across the organization, with clear financial and social impact goals tied to each intervention/initiative.
Those who report being further along — in a sustainable vs. a foundational or siloed stage of maturity — tend to stabilize investments in areas related to organizational setup, and place higher current prioritization or plan for increased investments in execution-oriented initiatives. An example for design and implementation of health equity initiatives vs. philanthropic funding demonstrates this trend.
Chart 5. Expected change in spending for two focus areas, by organizational health equity maturity
While investment is on the rise across the ecosystem, organizational annual revenue — and thus the inferred size of health equity-directed budget — frequently correlates to the scope and scale of health equity efforts. Organizations under $500 million in revenue are most likely to have established a health equity strategy within the last year and be at a foundational level of maturity. Roughly half of such organizations (53%) are currently focused on developing strategy and garnering leadership buy-in. Conversely, 70% of organizations with over $10 billion in revenue have advanced to delivering pilot programs and scaling health equity initiatives. They are also most likely to focus on increasing investment in technology and analytics solutions for health equity advancement.
Chart 6. Average scale of health equity prioritization, age and perceived maturity, by organizational size in annual revenue
Success factors and barriers
These investments seem to be paying off for many. The majority of organizations surveyed have observed a positive impact to their organization’s bottom line (65%) or to health outcomes (83%) over the past year. Organizations that have been able to quantify one or both of these improvements (46%) have identified leadership buy-in and community engagement and trust as their top success factors. Relatedly, community connectivity is one of the most common value dimensions driving organizational health equity support across the ecosystem (52%).
The majority observed a positive impact to their bottom line or to health outcomes over the past year as a result of health equity efforts.
When it comes to challenges, 2023 results highlighted a lack of common understanding or awareness of what health equity entails, financial commitment and dedicated resources as top barriers to health equity strategy enactment. The landscape has changed into 2024, with competing priorities emerging as a top challenge among respondents (41%) this year. A lack of financial commitment also persists for many organizations (36%). Notably, nearly a third of organizations (28%) point to the lack of an articulated business case for health equity as a barrier, with implications for financial investment into these initiatives.
Chart 7. Top three barriers and critical success factors in advancing health equity priorities
Health equity regulatory readiness
Health equity-related regulatory requirements are expanding into 2024, forcing providers, payers and life sciences organizations to develop new capabilities to meet and exceed evolving standards.
Considering new expectations from the Centers for Medicare & Medicaid Services, the National Committee for Quality Assurance (NCQA) and The Joint Commission, less than half of provider and payer organizations report being ready to meet requirements today. This trend points to significant work to come, as minimum health equity regulatory standards do not yet fully address the full set of clinical and social needs facing underserved populations. The areas of highest readiness today reflect core health care capabilities such as language access (48%) and health care access (47%), while areas for development such as social needs referral pathways (27%) and disparity root cause assessment (21%) reflect health care’s extension into the community. Although providers and payers exhibit similar levels of readiness across most categories, payers lead in perception of readiness for health literacy, access and coverage, while providers lead for designating a health equity leader. Of the organizations not ready today, most are developing or acting on a defined plan to enable readiness.
Providers, payers and life sciences organizations are developing new capabilities to meet expanding health equity regulatory requirements.
Chart 8. Reported readiness to meet health equity-related regulatory requirements (providers and payers only)
In the life sciences sector, expanding guidance from the Food and Drug Administration (FDA) now requires clinical trial diversity action plans to advance inclusive medical research. Overall, more organizations report they are ready to develop action plans today than activate them, reflecting the differing capabilities required for strategy vs. execution. Greater health equity maturity and organizational revenue correlate with increased readiness across both activities. In evolving toward more inclusive drug research and development, long-term strategies to build trust with underserved patient demographic groups will be critical, given that trust is currently a medium to high barrier for 58% of life sciences organizations.

Chapter 2
Leveraging data and technology to advance health equity goals
Data analytics is helping uncover health equity challenges and tailor interventions, with AI emerging as a critical tool in the process.
Capturing and analyzing data helps organizations understand what health equity challenges exist in which populations, design tailored interventions, measure program impact and drive accountability. Similar to 2023 results, most organizations collect and use health equity data to inform high-level strategic priorities but are not yet using analytics to drive and fine-tune health equity initiatives. More advanced technologies like generative AI are emerging as tools to advance practice, though most organizations are in the exploratory and learning phases of adoption.
Advanced technologies like generative AI are emerging as tools to advance health equity practice, though most organizations are in the exploratory and learning phases of adoption.
Data and analytics capabilities
Overall, organizations are inconsistent in data collection practices: 70% collect race/ethnicity and language (REaL) data, 57% collect information on social drivers of health (e.g., food security, housing stability, transportation access), 55% collect information on clinical outcomes by subpopulation (e.g., race/ethnicity, gender, geography), and 46% collect sexual orientation and gender identity (SOGI) data. As organizations seek to expand their health equity impact, there is room for improvement on collection, stratification and reporting of demographic and social needs measures so that interventions are tailored to identified health disparities. Trust will be an imperative enabler.
Some level of analytic capabilities (descriptive, diagnostic, predictive and/or prescriptive) are nearly universal (88% report using at least one), but descriptive analytics — the most basic form of data interactions — are most frequently used and yet only for a minority of organizations (47%).
While most organizations remain at an intermediate stage of health equity data maturity, a jump in organizations reporting that they are not currently building health equity data and analytics capabilities was observed from last year (3%) to this year (16%). Organizations that are earliest in their health equity strategic maturity and those with under $500 million in revenue most commonly fall in this category. In contrast, the higher-revenue organizations (over $5 billion) report being at the highest level of data maturity — using analytics to drive health equity improvement — more frequently than smaller organizations.
Across organizations, annual revenue and health equity strategy maturity appear to correlate to health equity data analytics capabilities.
Chart 10. Health equity data and analytics maturity stage by organizational annual revenue
The relative maturity of an organization’s health equity strategy appears to correlate to its health equity data analytics capabilities. Among organizations with sustainable health equity strategies, about half (49%) are driving improvement activities by leveraging health equity data, compared with just 8% of organizations with siloed health equity strategies.
Performance measurement and reporting
While the vast majority of organizations measure health equity-related metrics (93%) and report them internally (89%), lower frequency is seen for reporting externally (70%). Across the board, organizations are more likely to measure and report on an ad hoc basis vs. a consistent, defined cadence. More government organizations — particularly at the federal level — consistently report health equity metrics internally and externally, relative to other stakeholder groups. The findings suggest there are opportunities to improve the consistency of external data reporting, particularly among payers (20% on a consistent basis) and life sciences organizations (16% on a consistent basis).
Chart 11. Consistent vs. ad hoc external and internal reporting of health equity metrics, by segment
Role of generative AI
Most organizations report being in the early stages of considering the use of artificial intelligence (AI) in health equity initiatives — with particular interest for predictive analytics — although only a handful of organizations indicate already implementing AI-powered capabilities. Uncertainty was expressed about AI’s impact on the health industry, with potential ethical concerns around data bias and accuracy, as well as implementation challenges such as costs and training needs. Given the rapid evolution of AI technology and organizational understanding of its applications, adoption opportunities and barriers within each stakeholder group will be important to watch.

Chapter 3
Advancing health equity priorities by focusing on the workforce
High workforce competence boosts the impact of health equity initiatives amid varied DEI approaches.
Organizations report a moderate to high understanding of key health equity topics, with higher workforce competency correlated with quantifiable impact of health equity initiatives. Varied approaches to organizational diversity, equity and inclusion (DEI) may hold implications for health equity strategy activation.
There is a continued self-perception of a strong understanding of health equity context and drivers, however it is not translating universally into how and where to act.
Health equity education
Recent data shows progress in health equity competency: 2024 results indicated a 27% increase in organizations providing health equity training and education to their employees relative to 2023 findings.
Across organizations, there is a continued self-perception of moderate to high understanding of the definition and context of health equity, but knowledge of what health equity is does not universally translate into how and where to act. Close to half of government (46%) and nonprofit and community-based organizations (45%) perceive that their workforce actively practices a health equity mindset at a high rate, compared with lower rates among provider (29%), payer (27%) and life sciences organizations (21%). Organizations with higher confidence in their workforce’s use of a health equity mindset were more likely to report quantifiable clinical and financial impacts of their programs.
Chart 12. Perception of workforce’s health equity competency
Diversity, equity and inclusion
DEI efforts continue to be a critical enabler for many, with 57% of health industry organizations indicating that alignment with DEI objectives is driving internal prioritization of health equity activity. Across the United States, efforts to limit or bar DEI activities have surged within state legislatures and elevated to federal discourse, as exemplified by the recent U.S. Supreme Court decision to end affirmative action in higher education. As DEI is increasingly politicized, the related effect on support for health equity within health organizations will need to be monitored.
Many indicate that alignment with DEI objectives drives internal prioritization of health equity activity.
A majority (71%) evaluate workforce diversity as a factor in achieving their health equity goals. In contrast, just one in two provider organizations — and less than a third of single hospital locations or physician groups — evaluate internal policies and practices from an equity lens. Life sciences organizations are also nearly 20% less likely to assess employee diversity against consumer diversity, compared with some peer groups — although this appears to be a greater gap for pharma and medical device organizations than biotechs.
Chart 13. How organizations evaluate workforce diversity as a factor in achieving health equity goals
Various organizational structures for internal health equity and DEI functions exist, with near-equal proportions of organizations governing these activities under separate (32%) or as integrated departments (36%). While the findings suggest there is no one best approach, organizations reporting the highest level of health equity maturity were the most likely to have internal health equity and DEI departments integrated and aligned under one umbrella.

Chapter 4
Community, collaboration and policy impact health equity actions
Trust is key; the focus is growing on stigma reduction, affordability and language accessibility.
Respondents across stakeholder groups agree that effective health equity initiatives must anchor on the community, building and sustaining trust with consumers and beneficiaries across demographic groups.
Community-level access barriers
All stakeholders report tackling community-level access to care barriers, yet which barriers are being prioritized has shifted in the last year. Results from 2023 indicated that organizations were actively intervening to address the availability of providers, insurance coverage and culturally appropriate program and staffing, whereas 2024 data shows organizations shifting focus toward reducing health stigmas, mitigating financial barriers and improving language accessibility. One possible interpretation of these findings may be that organizations’ understanding of community barriers shifts as they mature from health equity aspiration to on-the-ground implementation.
Chart 14. Top areas of organization health equity focus related to community-level access barriers
Community and ecosystem partnerships
Aligned with 2023 findings, 2024 results point to high prioritization of community engagement as part of health equity advancement, though active engagement is not yet universal. Payers (67%), government (64%) and nonprofit organizations (60%) lead the way in seeking input and validation from community-based organizations and consumers as part of health equity strategy development. Across stakeholders, however, community-based organizations and consumers are less commonly engaged for health equity program design and delivery, presenting an opportunity for greater pull-through in the implementation process.
Community engagement continues to be a high priority within many organizations, though not universal.
Chart 15. Organizations seeking input from community-based organizations and consumers
Health industry organizations reaffirmed the significant value of ecosystem partnerships and collaboration to achieve their health equity goals. Today, organizations report frequently collaborating with others within their stakeholder segment: 81% of government organizations partner with other government organizations, 73% of providers with other providers, 61% of nonprofits with other nonprofits, 57% of payers with other payers and 56% of life sciences organizations with other life sciences organizations. Current cross-sector collaborations reflect the earlier prioritization seen in health care access and quality, as providers are the top external partner for payers, life sciences and government organizations. Similarly high rates of cross-sector partnerships are seen with government and nonprofit organizations, potentially reflecting a focus on expanding “last mile” reach and capabilities. An increase in cross-sector partnerships is expected across the full ecosystem, particularly with regard to less common areas of partnership today, such as with payers and life sciences organizations.
Chart 16. Active partnerships and future areas for increased focus
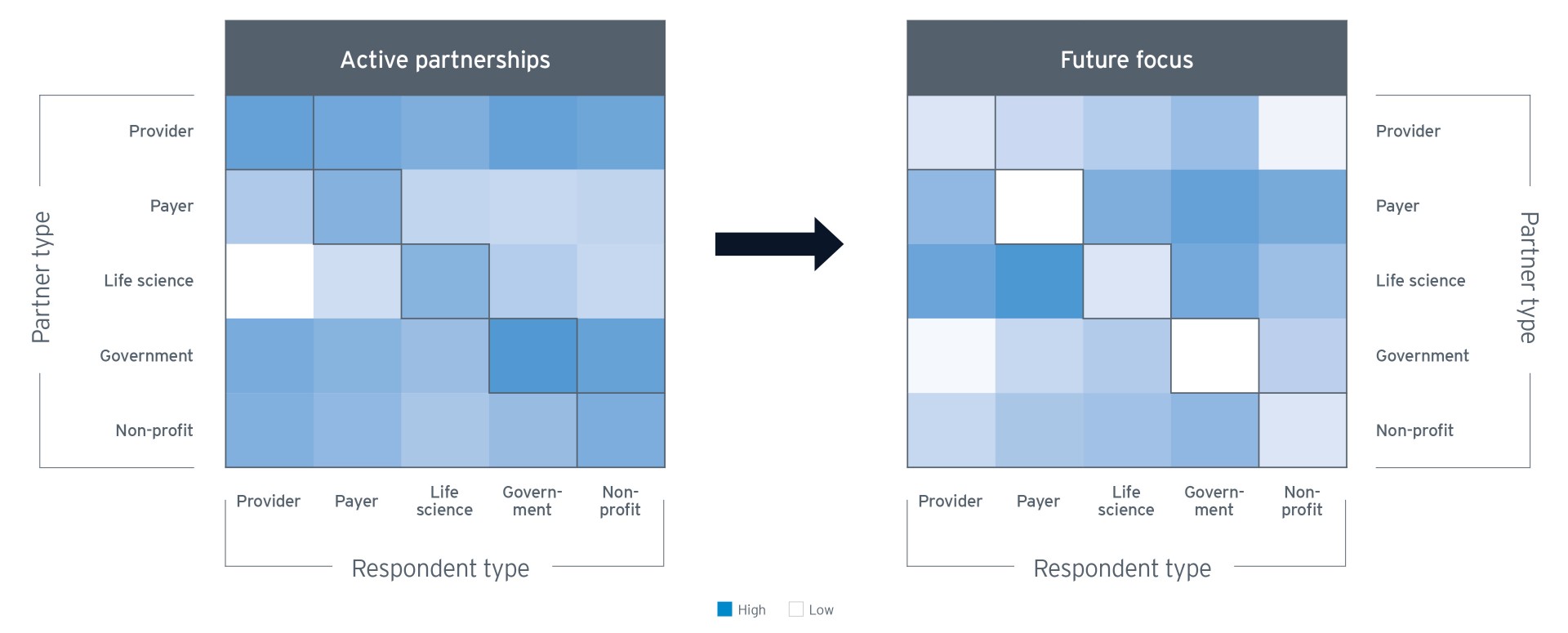
Health industry organizations reaffirmed the significant value of ecosystem partnerships and collaboration to achieve their health equity goals. Today, organizations report frequently collaborating with others within their stakeholder segment: 81% of government organizations partner with other government organizations, 73% of providers with other providers, 61% of nonprofits with other nonprofits, 57% of payers with other payers and 56% of life sciences organizations with other life sciences organizations. Current cross-sector collaborations reflect the earlier prioritization seen in health care access and quality, as providers are the top external partner for payers, life sciences and government organizations. Similarly high rates of cross-sector partnerships are seen with government and nonprofit organizations, potentially reflecting a focus on expanding “last mile” reach and capabilities. An increase in cross-sector partnerships is expected across the full ecosystem, particularly with regard to less common areas of partnership today, such as with payers and life sciences organizations.
Community engagement continues to be a high priority within many organizations, though not universal.
Summary: Strengthening health equity impact
Health equity remains a key focus across the health ecosystem, though practice and areas of prioritization continue to evolve. Investments continue in capacity building, technology and community engagement. While progress is underway, many organizations are not yet fully achieving goals or prepared to meet regulatory guidance on data capabilities, gap closures and outcomes. Variation within segments is often impacted by the economic scale of the organization involved, reflecting the resource gaps many smaller organizations have, compared with larger ones. With persisting disparities in health outcomes and a growing policy landscape emphasizing health equity activation, the field continues to move from health equity strategy development to impact delivery.
Key actions from EY's 2nd Annual Health Equity Survey:
- Share best practices and align efforts where possible to bridge resource gaps and build broader system-level capacity.
- Leverage the demonstrable business case for health equity to garner sustained leadership buy-in and financial commitment to health equity initiatives.
- Deploy expanded analytic capabilities to improve proactive identification and intervention for high-risk populations.
- Prioritize community engagement and trust-building throughout the end-to-end strategy development and execution process.
Moving forward, the EY Center for Health Equity will continue to explore what support each stakeholder segment — from payers, providers and life sciences to government and nonprofits — will need to launch programs, leverage technology and scale initiatives for broader impact.
The EY Center for Health Equity Team
Acknowledgments and contributions
The 2024 Health Equity Outlook Report was collaboratively written with notable contributions from Julie Nguyen, Kelly Hawk, Lauren Freeman, Lisa Goodin, Millka Baetcke, Rebeca Almeida and Sarah Brock of Ernst & Young LLP.
This edition of the Health Equity Outlook Report was published in March 2024
Get in touch with the EY Center for Health Equity
Like what you read? We’d like to hear from you.

