4. Sustainability
Future proofing smart hospitals and wider health systems means a whole lifecycle approach to the design and operations of facilities and services. Designing flexible and adaptable structures ensures that they remain fit for purpose over the long-term and not only reduces the need for constant upgrades but delays obsolescence. Energy use, lifecycle duration, pollution controls, and reducing carbon footprints all shape the architectural and technical design briefs for smart health facilities.
Moving to a hybrid care environment
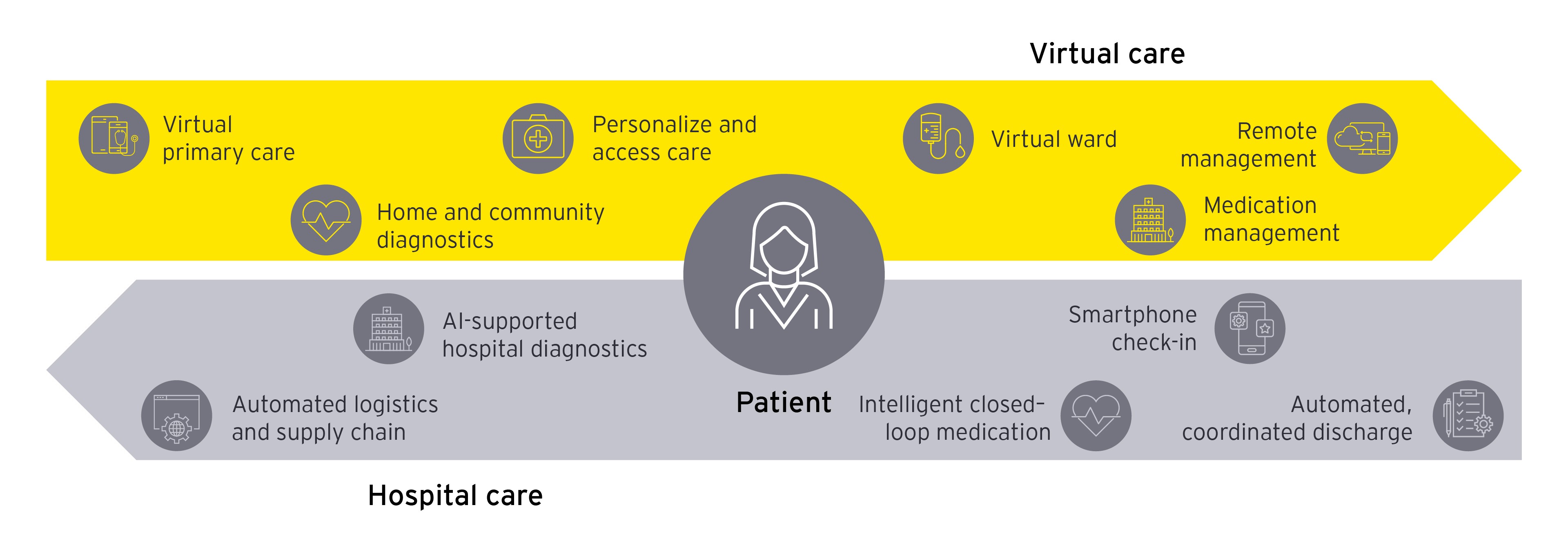
Virtual health alone can’t address the current challenges and drivers of health. It is the union between the physical and virtual worlds that will make a difference.
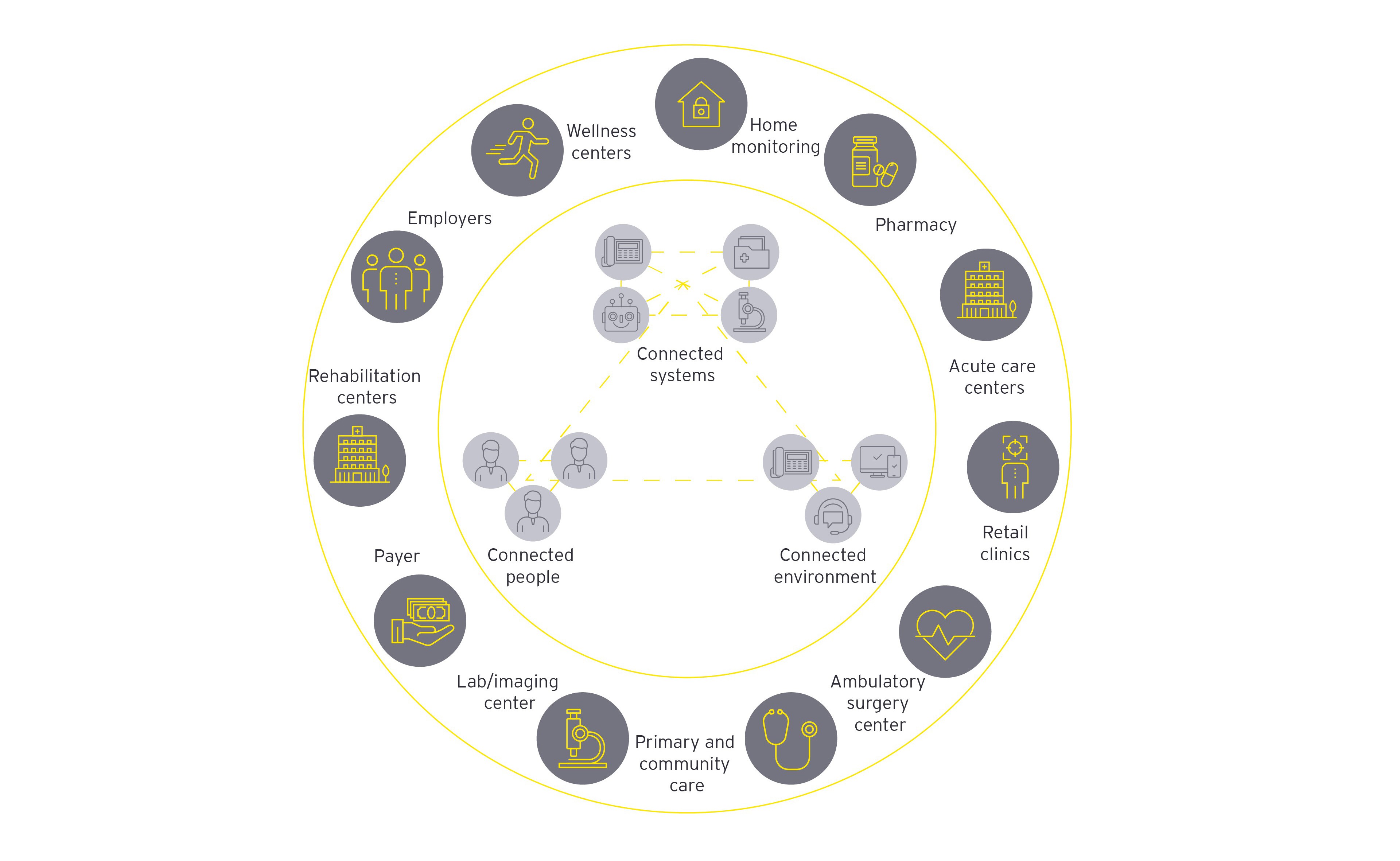
Becoming smart means integrating into the wider ecosystem and creating a virtual care platform that integrates data through interoperable patient record systems and digital enablers such as IoT, 5G, AI, and remote monitoring. To sustain and capture value faster in this new model, the organizational culture of health systems will need to transition toward a more agile and responsive model. For some health systems, this transition will be a complete organizational transformation. For others, this will be incremental, targeting efficiency and patient experience improvement through digital enablers.
It is abundantly clear that the future of health is smart and that advances in smart technology, smart algorithms and smarter care models will shape the way care is delivered and experienced. This new frontier will allow us to deliver the right insights, to the right people, at the right time, leading to smarter, better informed and more cost-effective care for providers and patients.
Contributors: Emily Mailes, Director, Health Consulting, Ernst & Young - New Zealand; Sheryl Coughlin, PhD, EY Global Health Sciences & Wellness Senior Analyst; Ankur Sadhwani, EY Global Health Analyst.