Integrated Care Systems (ICSs) tick all the right boxes—ideally providing equitable, well-connected and coordinated care across all aspects of a person’s health and social needs resulting in healthier populations and more sustainable systems. Supported by a contemporary and innovative information infostructure, ICSs could differentiate by enabling and sharing insights through data at scale. Read the full report (pdf).
In England, 42 ICSs now cover all areas and are the result of a steady shift in health policy over the past decade toward joining up of services to better meet the needs of local populations. Globally, similar policy interest can be seen in the desire for better integrating care and adapting care delivery through such things as patient-centered care, shared decision-making, medical homes and social prescribing.1,2,3 To unlock the power of ICSs as coordinated and collaborative ecosystems requires a new approach to health information architecture.
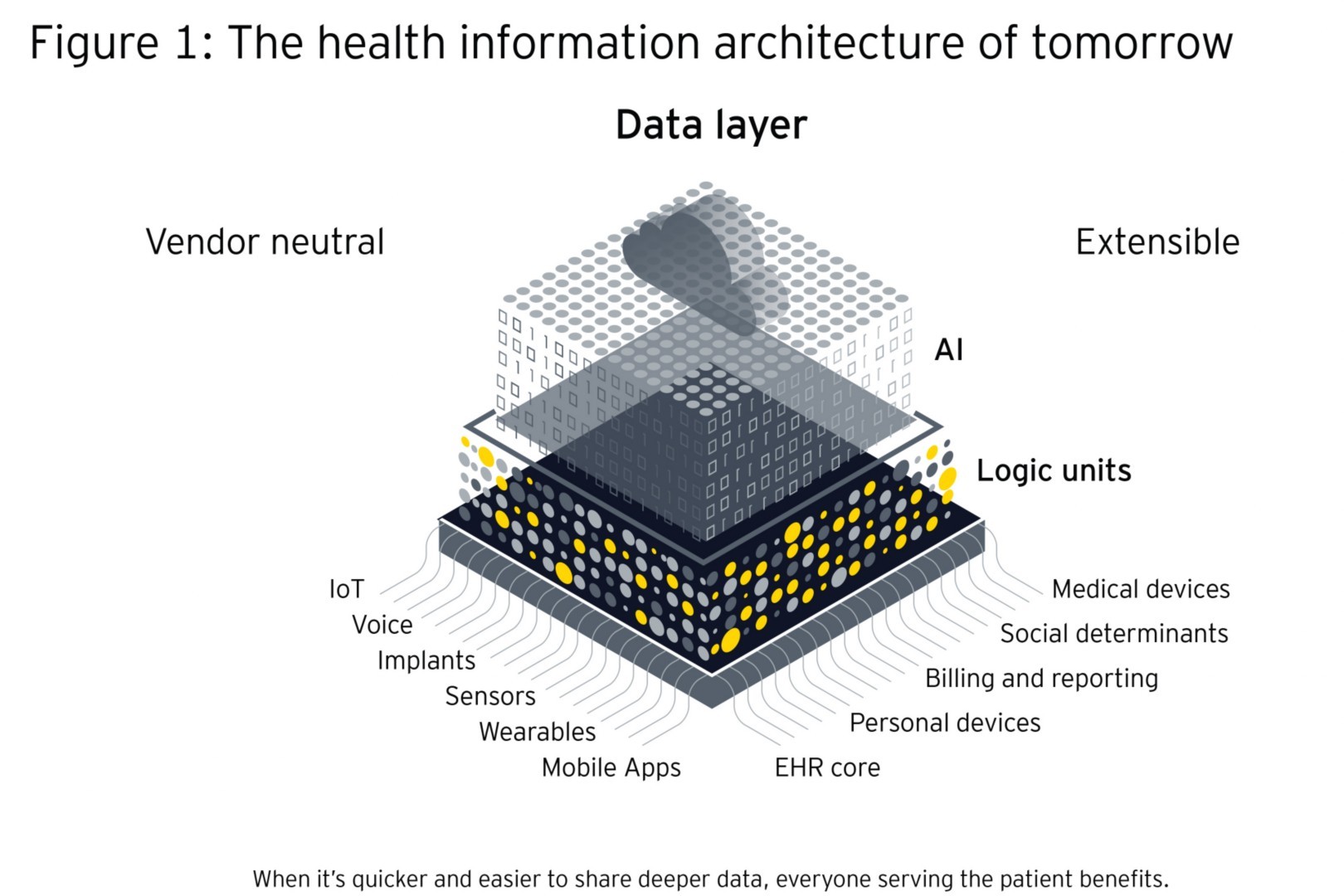
As data becomes the core asset of health and care, health systems cannot achieve their stated goals of improved wellness, sustainability and equity without an agile information infrastructure. Care systems that integrate health, social, community and local government services mean that thousands of people may need to access data for different purposes to coordinate care to meet a person’s health and social needs. These systems have the opportunity to remake their health information architectures into open platform environments that enable shared care records across the health journey, and allow emerging technologies to be applied to that infostructure to extract insights out of the data layer.
Such infrastructures also need to act as platforms of exchange. This means allowing the easy flow of data within, and among, systems and analytics capabilities that support the use of data for local needs, safely and securely.
Build for the future
Getting the information backbone of the integrated care ecosystem right is mission critical and infrastructure must be designed for the future, with the entire system in mind. This means sufficient flexibility to benefit from emerging technologies (e.g., artificial intelligence, augmented and virtual reality, hyper automation, decentralized identities, Web 4.0, and digital twins), digital-first consumer and workforce experiences, and the capability to integrate within a national and or multinational system(s).
The future vision should be of systemically and semantically architected open systems, built from an ecosystem mindset, that accommodate a plurality of approaches and information needs. This should be a dynamic infrastructure, where data is captured in a smart way, adheres to a shared semantic standard tailored to the specific use case and moves data through modern interfaces like RESTful web application programming interfaces (APIs). In this infrastructure, health data captured in electronic patient records (EPRs) will need to be able to flow through this standards-based information backbone, either directly integrating with the backbone API or by publishing their vendor-controlled data objects in a format that can be mapped against it, like HL7 FHIR that is designed for extracting data.
All three largest Nordic vendors of Electronic Health Record (EHR) systems in Norway (DIPS), Sweden (Cambio) and Finland (TietoEvry) and the largest vendor of EHRs for elderly care providers in the Netherlands (Nedap) use a vendor neutral data repository based on openEHR.4 Dedalus, a supplier of clinical and diagnostic solutions in many European countries has recently committed to openEHR.5
The system should be federated, where the architecture is one of multiple interconnected nodes and shared principles, governance and open standards. Such an architecture allows shared infrastructure services to scale incrementally over time, links different domains together and provides the means to share sensitive health data safely and securely. If built on an open hybrid cloud platform that mixes on-site and third-party cloud computing infrastructure, standard functions such as patient identity management, and verification can be provided nationally while allowing for locally-led workstreams and applications.
Build on the installed base
Few opportunities exist for greenfield sites, therefore new uses and users must be interwoven with the pre-existing built environment, the installed base. The primary strategic question facing integrated delivery system decision makers now is how to best build scale with sustainable technology choices that suit both national and local purposes. Considerations include the installed base, required enabling infrastructure, as well as future care model and infrastructure needs. Recently reported, is the decision of a Florida-based health care system to spend US$65m to switch from one monolithic EHR system to another to allow access to patient records irrespective of location.6 The cost of switching from one siloed system to another is something that few can afford. It begs the question as to whether health systems should continuously switch or change as needs evolve or if they might choose to work with a vendor-neutral data layer instead?
Three building blocks to create the right environment
Creating the right environment for integrated care systems to thrive will be built upon the information architecture, core features, and shared common terminology and standards.
1. Infostructure information architecture
For a truly integrated system, a data environment with no connection restrictions other than permissions and security is needed. This, in turn, necessitates an open platform architecture that allows for the storage and linking of structured and unstructured data, and that determines how data flows. A decentralized and networked infrastructure will unify disparate information from multiple sources and make sense of it. This means capturing and linking all relevant data regardless of where it is created and stored.
The optimal platform separates content and technology and will be vendor-neutral, distributed and modular — incorporating third-party as well as legacy systems. It provides a stabilizing framework for maintaining governance mechanisms which include standards, interfaces and rules. The architecture should be separated into different layers that organize transactions and interactions: the data layer, the application layer and the logic layer:
- The data layer is standardized in terms of format, nomenclature, terminologies and definitions, which allows it to flow into other systems.
- The application layer requires a fully systemic design of workflow based upon triggered events of care or intervention, e.g., clinical workflows.
- The logic layer contains sets of rules that define boundaries and exceptions, and can form workflows.